Blogs Zynova
- admin
- 0 Comments
What Is Robotic Surgery? How It Works, Who Is Eligible & Is It Safe?
Understanding Robotic Surgery Robotic surgery, also called robotic assisted surgery, is an advanced surgical technique where doctors use a robotic system to perform complex procedures with high precision and control. Despite the name, the robot does not operate on its own. The surgeon remains fully in control at all times. In simple words, robotic surgery is a modern form of minimally invasive surgery that allows surgeons to operate through small cuts using robotic arms guided by a computer system. Over the last decade, robotic surgery in Mumbai and worldwide has grown rapidly. Patients prefer it because it offers less pain, smaller scars, faster recovery, and better surgical accuracy compared to traditional open surgery. With the growing demand for advanced surgery in India, especially in cities like Mumbai, more hospitals are adopting robotic surgical technology. However, choosing the right hospital and experienced robotic surgeon is extremely important for safety and results. What Is Robotic Surgery? Definition of Robotic-Assisted Surgery Robotic surgery, also known as robotic assisted surgery, is an advanced form of minimally invasive surgery in which a specially trained surgeon uses a robotic system to perform complex surgical procedures with enhanced precision, flexibility, and control. In robotic surgery, small surgical instruments are attached to robotic arms, which are controlled entirely by the surgeon from a computerized console. The system provides high-definition, 3D magnified vision and allows extremely precise movements that are often beyond the capability of the human hand alone. Robotic surgery represents one of the most significant advancements in modern and advanced surgery, improving outcomes across multiple specialties. Does the Robot Operate Independently? No, the robot does not operate independently. One of the most common misconceptions about robotic surgery is that the robot performs the surgery on its own. This is not true. In robotic assisted surgery, the surgeon remains in complete control throughout the procedure. The robotic system does not: Make decisions Move without instruction Replace the surgeon Instead, it translates the surgeon’s hand movements into smaller, more precise movements inside the patient’s body. If the surgeon stops, the robot stops immediately. Difference Between Robotic Surgery and Automated Surgery Robotic surgery is often confused with automated surgery, but they are very different. Automated surgery: Machines function independently using programmed instructions. Robotic assisted surgery: The surgeon controls every action in real time. Robotic surgery enhances human skill — it does not replace human expertise. The technology serves as an extension of the surgeon’s hands, eyes, and precision. Role of the Surgeon in Robotic Procedures During robotic surgery, the surgeon: Sits at an advanced control console Views a magnified 3D HD image of the surgical area Controls robotic arms using hand and foot controls Performs delicate surgical steps with high precision The robotic system filters out natural hand tremors and enhances fine movements. However, every movement originates from the surgeon. This combination of human expertise and robotic precision improves surgical accuracy, reduces complications, and enhances patient outcomes. Evolution of Robotic Surgery Surgery has evolved dramatically over the past century. 1. Open Surgery Traditional open surgery required large incisions. Although effective, it involved: More blood loss Higher infection risk Longer hospital stays Slower recovery 2. Laparoscopic Surgery Laparoscopic (keyhole) surgery introduced smaller incisions and camera guidance. It reduced recovery time but had limitations such as: Limited range of motion 2D visualization Restricted instrument movement 3. Robotic Surgery Technology Robotic surgery was developed to overcome these limitations. It offers: 3D high-definition vision Greater instrument flexibility Enhanced dexterity Improved precision Today, robotic surgery in India is expanding rapidly across orthopaedics, urology, gynaecology, and oncology. Globally, robotic assisted surgery is becoming the preferred option for many complex and minimally invasive procedures. How Does Robotic Surgery Work? (Step-by-Step) Understanding how robotic surgery works helps patients feel informed and confident. 1. Pre-Operative Planning Before surgery, doctors conduct: Blood investigations CT scans or MRI Detailed imaging studies Physical examination These tests help create a precise surgical plan tailored to the patient. 2. Anaesthesia The patient is given general anaesthesia so they remain asleep and pain-free during the procedure. 3. Small Incisions Instead of a large cut, the surgeon makes small incisions (usually 1–2 cm). 4. Insertion of Robotic Arms Robotic arms equipped with tiny surgical instruments are inserted through these small cuts. 5. 3D HD Camera Vision A high-definition camera provides a magnified 3D view, sometimes up to 10 times magnification. This allows the surgeon to see delicate structures clearly. 6. Surgeon-Controlled Movements The surgeon controls the robotic arms from a console. The system translates large hand movements into micro-movements inside the body, ensuring: Higher precision Better stability Minimal tissue damage Reduced bleeding What Does the Robot Actually Do During Surgery? The robotic system enhances surgical performance by: Improving precision and control Filtering out hand tremors Allowing 360-degree wrist rotation Operating in tight and hard-to-reach areas Increasing surgical consistency It does not replace the surgeon. Instead, it acts as a highly advanced surgical assistant. Types of Surgeries Performed Using Robotic Technology Robotic surgery applications are growing rapidly in India and worldwide. 1. Orthopaedic Robotic Surgery Robotic hip replacement surgery Robotic knee replacement Robotic spine surgery Robotics helps ensure accurate implant positioning and joint alignment. 2. Gynaecology Robotic Surgery Robotic hysterectomy Fibroid removal Endometriosis surgery 3. Urology Robotic Surgery Robotic prostate surgery Kidney tumor removal Bladder reconstruction 4. Cancer and General Surgery Colorectal cancer surgery Gastrointestinal surgery Lung surgery Robotic surgery in cancer care improves tumor removal precision while preserving healthy tissue. Who Is Eligible for Robotic Surgery? Robotic surgery eligibility depends on multiple factors. Ideal Candidates: Patients requiring minimally invasive procedures Early-stage cancer patients Joint replacement patients Patients seeking faster recovery Factors Doctors Evaluate: Age Overall health condition Disease stage Complexity of surger Previous surgical history A detailed medical evaluation determines whether robotic assisted surgery is suitable. Who May Not Be Suitable for Robotic Surgery? Certain patients may not be ideal candidates: Emergency surgical cases Severe heart or lung disease Extremely advanced disease High surgical risk patients Final decision is always made after thorough consultation with
- admin
- 0 Comments
Comprehensive Oncology Care: Diagnosis, Treatment & Follow-Up Under One Roof
Why Comprehensive Oncology Care Is the Need of Today Cancer is no longer a rare disease. In the global community, and especially in India, the incidence of cancer is rising at an alarming rate due to lifestyle changes, pollution, the use of tobacco products, and the aging population. Now it is one of the most common causes of deaths worldwide. With modern medical advancements, early detection and timely treatment can significantly improve survival. However, patients can benefit from these advances only when they have access to comprehensive oncology care. Many patients face challenges because cancer treatment is scattered across different hospitals. They may visit one center for diagnosis, another for surgery, and a third for chemotherapy or radiation therapy. This fragmented approach often results in: Delays in diagnosis Poor coordination between doctors Repeated tests and higher expenses Emotional stress for families “Under one roof” means a fully integrated cancer treatment center where diagnosis, treatment, supportive care, and follow-up happen in the same place. This structured model improves treatment accuracy, enhances survival rates, and ensures a smoother patient experience. A modern cancer treatment center in Mumbai offering integrated services allows patients to receive seamless care without losing valuable time. Comprehensive care ensures coordinated, timely, and precise cancer management. What Does “Comprehensive Oncology Care” Actually Mean? Comprehensive cancer care refers to complete, end-to-end cancer management. It covers every stage of the patient journey, including: Detection → Diagnosis → Staging → Treatment Planning → Active Treatment → Recovery → Follow-Up → Survivorship Unlike standalone facilities that provide only chemotherapy or surgery, a fully integrated oncology hospital offers multidisciplinary cancer care supported by advanced technology and expert coordination. Key Components of Complete Cancer Care Early cancer detection and screening Accurate cancer diagnosis and staging Personalized oncology treatment plans Advanced cancer treatment options Cancer supportive care Palliative cancer care Long-term cancer follow-up care Technology such as PET-CT scans, molecular testing, and genetic profiling improves diagnostic precision and allows doctors to monitor response continuously. Multidisciplinary Oncology Team: Backbone of Comprehensive Cancer Care Cancer is complex. One doctor alone cannot manage every aspect of diagnosis and treatment. That is why a cancer specialist’s team, also known as a tumor board, plays a critical role. During tumor board meetings, specialists review imaging reports, biopsy test results, staging details, and the patient’s overall health before finalizing the best cancer treatment plan. Specialists Involved in Multidisciplinary Cancer Care Medical Oncologist Manages chemotherapy, targeted therapy, immunotherapy, and hormone therapy. Monitors response and handles chemotherapy side effects. Surgical Oncologist Performs tumor removal surgeries, organ-preserving procedures, minimally invasive surgeries, and reconstructive cancer surgery. Radiation Oncologist Plans and delivers radiation therapy using precision techniques while protecting healthy tissues. Pathologist Confirms cancer diagnosis, determines tumor grading, and performs molecular testing. Radiologist Interprets CT scan, MRI, and PET-CT imaging to detect and monitor disease progression. Onco-nurses, Nutritionists, Psychologists, and Rehabilitation Experts Provide cancer supportive care, nutritional guidance, emotional counseling, and recovery support. This team-based approach ensures personalized and precise cancer patient care. Step-by-Step Oncology Care Under One Roof 1. Early Cancer Detection & Screening Early cancer detection significantly improves survival rates. Unfortunately, many patients ignore early cancer symptoms, such as: Persistent lumps Unexplained weight loss Continuous fatigue Abnormal bleeding Chronic cough Change in bowel habits Importance of Cancer Screening Regular cancer screening programs help detect cancer before symptoms appear. Common screening programs include: Breast cancer screening Cervical cancer screening Oral cancer screening Prostate cancer screening Colorectal cancer screening High-risk individuals, including those with family history or tobacco use, benefit greatly from routine screening. Benefits of Early Detection Less aggressive treatment Shorter recovery time Higher survival rates Reduced financial burden Better quality of life 2. Accurate Cancer Diagnosis & Staging An accurate cancer diagnosis forms the foundation of effective treatment. Diagnostic Process Includes the Following: Imaging Tests CT scan MRI PET-CT Biopsy Test Confirms cancer type Determines tumor characteristics Histopathology & Molecular Testing Identifies genetic mutations Guides targeted therapy Blood Tests & Tumor Markers Monitor disease progression Cancer Staging (Stage I–IV) Cancer staging determines how far the cancer has spread. Early-stage cancers may require surgery alone, while advanced stages may need combination therapy. Correct staging ensures the right personalized cancer treatment plan. 3. Personalized Cancer Treatment Planning Every patient is different. Personalized cancer treatment considers: Cancer type and stage Tumor biology Patient’s age and medical condition Genetic and molecular profile Patient preferences Doctors follow evidence-based clinical guidelines to design a customized oncology treatment plan. Continuous evaluation ensures treatment adjustments when necessary. Advanced Cancer Treatment Options Available Under One Roof A comprehensive oncology hospital provides all major cancer treatment options in one location. Medical Oncology Chemotherapy Destroys fast-growing cancer cells and prevents spread. Targeted Therapy Focuses on specific cancer-causing genetic mutations. Immunotherapy Strengthens the immune system to fight cancer. Hormone Therapy Used for hormone-sensitive cancers such as breast and prostate cancer. Surgical Oncology Tumor removal surgery Organ-preserving cancer surgeries Minimally invasive techniques Robotic-assisted surgery Reconstructive procedures Radiation Oncology External beam radiation therapy Intensity-Modulated Radiation Therapy (IMRT) Image-Guided Radiation Therapy (IGRT Combination therapies (surgery + chemotherapy + radiation therapy) often improve survival and long-term outcomes. Patients seeking oncology treatment in Mumbai benefit from access to these advanced technologies within an integrated oncology hospital. Supportive Care: Managing Side Effects & Improving Quality of Life Cancer treatment may cause: Fatigue Nausea Hair loss Pain Low immunity Emotional distress Cancer supportive care focuses on improving comfort and managing chemotherapy side effects through: Pain management programs Nutritional counseling Psychological therapy Infection control guidance Physical rehabilitation Holistic care improves treatment tolerance and quality of life. Palliative Care: Comfort, Dignity & Symptom Relief Palliative cancer care supports patients at any stage of illness. It is not limited to end-of-life situations. Services Include: Advanced pain management Symptom control Emotional and psychological support Family counseling Support during advanced cancer treatment Early integration of palliative care enhances comfort and dignity. Follow-Up Care & Cancer Survivorship After active treatment, structured cancer follow-up care is essential. Follow-Up Includes: Regular scans Blood tests Physical examinations Monitoring for recurrence Cancer Survivorship
- admin
- 0 Comments
Exercises After Knee Replacement: A Complete Guide for Faster Recovery
Taking care of yourself and being patient will help you heal after knee replacement surgery. The surgery will help with pain and movement, but the real success of the procedure depends on how well you stick to your recovery plan, especially the exercises you do after knee replacement. Our orthopedic specialists at Zynova Shalby Hospital always stress that physiotherapy and simple daily exercises are just as important as the surgery itself. These movements will help your knee get stronger, become more flexible, and make it easier for you to get back to your normal life. Why Are Exercises Important After Knee Replacement? A lot of people think that just resting after surgery is enough, but that’s not true. If you don’t do your exercises, your knee can get stiff and weak, which will make it take longer and hurt more to heal. Regular rehabilitation exercises after knee replacement are crucial because they: Make blood flow better and stop clots from forming. Make the joint less swollen and stiff. Strengthen the muscles around the knee to give it more support. Get back your balance and ability to walk. Make sure your new knee joint lasts a long time. When Can You Start Exercises After Knee Replacement? Most patients can start moving around gently within 24 hours of surgery with the help of a physiotherapist. As you get better, the routine gets better: Weeks 1–3: Exercises to improve flexibility and range of motion. Weeks 4–6: Practice walking and getting stronger. After six weeks: Activities that don’t put too much stress on your body to build endurance. Before starting or changing your exercise plan, always listen to what your doctor says. Best Exercises After Knee Replacement Here are some safe and effective exercises that our experts at Zynova Shalby Hospital often recommend: 1. Pumps for the Ankles : Put your back flat on the ground. Move your ankle up and down slowly, like you’re pressing and releasing a pedal. Do it again 10–15 times. Helps with swelling and better blood flow. 2. Sets for the quadriceps : Sit with your leg straight on the bed. Tighten your thigh muscles and push the back of your knee downwards. Hold for 5–10 seconds, then relax. Builds thigh strength and improves knee stability. 3. Heel Slides : Lie on your back with legs stretched. Slowly slide your heel toward your hip, bending the knee. Hold for a few seconds, then straighten the leg. Improves flexibility and bending ability. 4. Straight Leg Raises Lie down with the operated leg straight and the other bent. Lift the operated leg about 6–12 inches from the bed. Hold for 3–5 seconds, then lower slowly. Strengthens thigh and hip muscles without stressing the knee. 5. Knee Bends (Seated or Standing) Sit on a chair or stand with support. Bend your operated knee gently as far as it feels comfortable. Return slowly to the starting position. Strengthens thigh and hip muscles without stressing the knee. 6. Walking Begin with a walker or crutches. Take short, slow steps. Gradually increase your walking distance each day. Improves mobility, endurance, and overall confidence in using your new knee. Safety Tips While Doing Exercises While these exercises are safe, precautions are always important: If you experience severe pain, stop (some discomfort is normal). Steer clear of high-impact exercises like jumping and running. Exercise on a level, secure surface at all times. Utilize assistance as soon as possible. Never miss a follow-up appointment with your physiotherapist. Long-Term Exercises for Knee Health Once your recovery is complete, you can adopt low-impact exercises to keep your knee strong and flexible: Swimming – Gentle and effective without putting weight on the knee. Cycling – Builds strength and range of motion. Yoga and stretching – Enhances flexibility and balance. Light strength training – Keeps muscles strong for joint support. Conclusion Recovery from knee replacement surgery is a process that requires patience, and exercising is the most important step in the process. Exercising after knee replacement makes a person feel better, more comfortable, and confident to perform daily activities again. At Zynova Shalby Hospital in Ghatkopar, Mumbai, we feel that surgery is just half the process of recovery; complete rehabilitation is equally essential. Our experienced orthopedic surgeons and physiotherapy staff work closely with every patient to develop exercise programs that are both secure and efficient, promoting faster recovery and better long-term results. FAQs 1. When can I start exercises after knee replacement surgery? You can begin light exercises such as ankle pumps and thigh contractions within 24 hours after surgery, under the guidance of a physiotherapist. 2. What exercises should I avoid after knee replacement? Avoid high-impact activities like running, jumping, or heavy weightlifting, as they can strain your new knee joint. Stick to low-impact exercises recommended by your doctor. 3. Can I climb stairs after knee replacement surgery? Yes, but only after a few weeks and with proper guidance. Initially, use support and take one step at a time until your muscles are stronger.
- admin
- 0 Comments
Top 3 Most Common Types of Cancer in Women You Should Know
Introduction Did you know that cancer is one of the biggest health problems for women all over the world? But most of the time, it can be treated or stopped when it is found early. Sadly, most women don’t pay attention to the early signs because they think they’re just small health problems. The first step in protecting your health is to learn about the different kinds of cancer that can affect women. Being aware early on can literally mean the difference between life and death for people with breast cancer, cervical cancer, skin cancer, or ovarian cancer. Top 3 Most Common Types of Cancer in Women Cancer continues to pose a great danger to the health of women globally. Some of the most frequent forms of cancer in women include breast cancer, cervical cancer, and skin cancer. Let us get into detail about each of these forms of cancer in women, the signs they warn of, and why early diagnosis matters so much. Breast Cancer – It happens when breast cells divide and multiply too quickly and form a mass or tumor. The disease usually starts in the milk ducts or lobules, but if it isn’t treated, it can spread to other parts of the body. Breast cancer is the most common type of cancer in women around the world. The good news is that it can be found early if the patient does self-exams and mammograms on a regular basis. Warning Signs of Breast Cancer: A lump in the breast or underarm Alterations in the shape or the size of the breast Abnormal nipple discharge Skin dimpling or redness on the breast Why Early Detection of Breast Cancer is Vital: Breast cancer boasts one of the best survival rates if found early. Screening mammograms and regular self-examinations are lifesavers that identify abnormalities early, when they are not yet able to metastasize. Tips For Preventing Breast Cancer: Have a healthy weight and be physically active Reduce alcohol intake Breastfeed if possible Pay attention to your family’s health history Cervical Cancer – The cervix, the lower part of the uterus near the vagina, is where cervical cancer starts. Persistent human papillomavirus (HPV) infection is the main cause. Routine Pap smears and HPV testing detect it even before it manifests as cancer because it typically starts as precancerous abnormalities. Warning Signs of Cervical Cancer: Abnormal bleeding (perimenstrual, after intercourse, or after menopause) Abnormal vaginal discharge Pain during intercourse or pelvic discomfort Why Screening Matters for Cervical Cancer: Most cervical cancers arise because women do not attend routine Pap smears or HPV tests. Early detection of precancerous characteristics greatly improves the success of treatment. How to Prevent Cervical Cancer: Get the HPV vaccine. HPV infection is the main cause of cervical cancer, so getting the vaccine can greatly lower your risk. Regular Pap Smears and HPV Testing: Pap smears can find changes in the cervix that aren’t normal before they turn into cancer, and HPV testing can find infections early. When you’re intimate, be safe. Using protection can help lower your risk of getting HPV. Stop smoking. Smoking weakens the immune system, which makes it harder for the body to fight HPV infections. Cervical cancer is different because it can be found before it becomes cancer, which makes it very easy to stop. Women should never miss their regular screenings because the best way to protect themselves is to find problems early. Skin Cancer in Women Another of the most prevalent cancers in women is skin cancer, which is mostly brought on by exposure to ultraviolet (UV) radiation from tanning beds or the sun. Skin cancer can strike anyone, but it is more likely to strike women who spend a lot of time outside without protection. Melanoma is the most aggressive of its types, whereas squamous and basal cell carcinomas are more prevalent but less difficult to treat. Warning Signs of Skin Cancer New moles or growths that change in shape, size, or color Sores or wounds that persist Rough, red, or scaly skin patches Itching, bleeding, or mole pain One helpful method for spotting melanoma is the ABCDE rule: A – Asymmetry: The mole’s two halves are not identical Border: Uneven or hazy edges Color: Various tones of red, black, or brown Diameter: More than 6 mm Evolving: Any change in size, color, or shape Importance of Early Detection and Regular Screenings The most important thing that connects breast cancer, cervical cancer, and skin cancer is the fact that all of them can often be detected early. Regular screenings, health check-ups, and self-examinations allow women to identify unusual changes in their bodies before they turn into serious problems. Preventive healthcare should never be ignored, as early intervention improves survival rates significantly. Women must also be aware of their family medical history, lifestyle factors, and environmental risks. For example, if breast cancer runs in your family, mammograms may need to start earlier than the general recommendation. Similarly, if you are frequently exposed to the sun, protecting your skin should be a daily habit. General Tips to Reduce Cancer Risk in Women You can’t stop all cancers, but you can lower your risk a lot by making smart choices about your health: Eat a balanced diet that includes whole grains, fruits, vegetables, and lean proteins. Stay active: You should work out for at least 30 minutes most days of the week. Don’t smoke and drink only in moderation. Use sunscreen and stay away from tanning beds to protect your skin from the sun. Get your shots: One of the best ways to avoid cervical cancer is to get the HPV vaccine. Get regular checkups and screenings for your health. Conclusion Cancer is a word that can cause fear, but knowledge and early detection can save lives. The top 3 most common types of cancer in women – breast cancer, cervical cancer, and skin cancer – can often be prevented or successfully treated if identified early. By paying attention to warning signs,
- admin
- 0 Comments
Heart Bypass Surgery Recovery Time: Essential Tips for a Faster and Smoother Recovery
Introduction Heart bypass surgery, which is also known by coronary artery bypass grafting (CABG), is a highly common surgery that is performed to restore blood flow into the heart when the arteries are blocked or narrowed. Even though surgery itself is a milestone, patients and their families are equally concerned about what happens after the recovery period. Education on recovery time after bypass surgery on the heart, precautions, and what one can expect during each stage of recovery is key in ensuring a problem-free and safe recovery. At Zynova Shalby Hospital, patient education is highly valued, and an educated patient recovers better. This blog is intended to guide you through each stage of recovery after bypass surgery, timeline, advice on care, limitations, and when to watch out for medical attention. What is Bypass Surgery Bypass surgery, or coronary artery bypass grafting (CABG), is a surgical procedure intended to improve blood flow into the heart. It is usually recommended for people who have severe coronary artery disease, where the coronary arteries that feed blood into the heart are blocked or narrowed by plaque buildup. During surgery, doctors take a healthy blood vessel from another part of the body—most often the leg, arm, or chest—and attach it to the heart. This new vessel creates a “bypass” around the blocked artery, ensuring oxygen-rich blood can continue flowing to the heart muscle. The procedure is highly effective in easing chest pain (angina), improving stamina, and lowering the risk of a heart attack in patients with significant blockages. It is generally suggested when lifestyle changes, medication, or less invasive procedures like angioplasty are not enough to restore circulation. How Long is the Recovery Time After Bypass Surgery? Recovery after bypass surgery happens gradually and can differ for each person depending on their age, overall health, lifestyle, and the number of grafts done. On average: Hospitalization: Most patients remain in the hospital for about 5–7 days after surgery. Early Recovery (First 6–8 Weeks): This stage focuses on regaining mobility, strength, and independence. Full Recovery: It may take around 3–6 months for the body to completely heal and for energy levels to return to normal. Remember, recovery does not only mean physical healing but also regaining emotional strength and confidence. What to Expect in First Weeks In the early days, patients may notice: Chest discomfort after bypass surgery due to healing of the breastbone. Swelling or soreness at the incision site or in the leg (if veins were taken from there). Tiredness and low energy as the body focuses on recovery. Mood changes or anxiety, which are normal after major surgery. It’s important not to panic if you feel chest pain after bypass surgery, as mild discomfort is part of the healing process. However, severe or persistent pain should always be reported to your doctor. Essential tips for faster recovery of Bypass Surgery Follow Medical Advice Strictly Your healthcare team will provide specific instructions about medications, wound care, and lifestyle changes. Taking your prescribed medicines on time helps prevent complications like infections, blood clots, or irregular heartbeat. Pay Attention to Wound Care Incision care is one of the most important aspects of after bypass surgery care. Keep the surgical site clean and dry. Watch out for signs of infection such as redness, swelling, or unusual discharge. Manage Pain Effectively It’s natural to have some chest discomfort after bypass surgery. Taking prescribed painkillers and practising relaxation techniques can make recovery easier. Avoid over-the-counter medication unless your doctor approves. Gradual Physical Activity Walking is the best form of exercise during the recovery phase. Begin with short walks and slowly increase duration and intensity as advised. Physical therapy or a cardiac rehabilitation program plays a big role in rebuilding strength and stamina. 5. Monitor Your Diet Carefully A heart-healthy diet is vital for recovery and long-term well-being. Include fresh fruits, vegetables, whole grains, lean proteins, and healthy fats. Reduce salt, sugar, and saturated fats to support heart function and prevent future blockages. 6. Sleep and Rest Well Adequate rest speeds up bypass surgery recovery time. Sleep may be challenging initially due to discomfort, but using pillows for support and practicing relaxation before bedtime can help. 7. Emotional Healing Matters It’s common to feel low or anxious after heart surgery. Joining support groups, practicing meditation, or counseling can help patients cope better with post-surgery emotional stress. Precautions after bypass surgery Taking the right *precautions after bypass surgery* ensures long-term benefits and prevents setbacks: Avoid Heavy Lifting: Refrain from lifting anything heavier than 2–3 kg for the first few weeks. No Driving Initially: Patients should avoid driving for at least 4–6 weeks or until cleared by their doctor. Careful with Stairs: Use support when climbing stairs in the early stages. Avoid Smoking & Alcohol: Both can slow recovery and increase the risk of complications. Regular Monitoring: Keep track of blood pressure, blood sugar, and cholesterol levels. Lifestyle Changes for Long-Term Recovery Bypass surgery not only saves lives but also offers a second chance to build a healthier lifestyle. Here are a few long-term habits to adopt: Regular exercise (walking, cycling, yoga as permitted). Stress management through meditation or breathing exercises. Heart-friendly diet low in cholesterol and trans fats. Regular medical checkups and adherence to prescribed medications. Conclusion Heart bypass surgery is a major milestone, but recovery can be smooth and successful with the right care and guidance. While every patient’s healing journey is unique, following precautions, recognizing early warning signs, and making necessary lifestyle changes are key to regaining strength and returning to an active life. At Zynova Shalby Hospital, Ghatkopar, our team of expert cardiologists and cardiac surgeons go beyond surgery—we walk with you through every stage of recovery. With advanced technology, personalized rehabilitation, and compassionate care, we are dedicated to helping you and your loved ones live healthier, stronger, and longer lives. If you or someone close to you is preparing for bypass surgery, choose Zynova Shalby Hospital for trusted expertise, complete heart care, and a recovery journey you
- admin
- 0 Comments
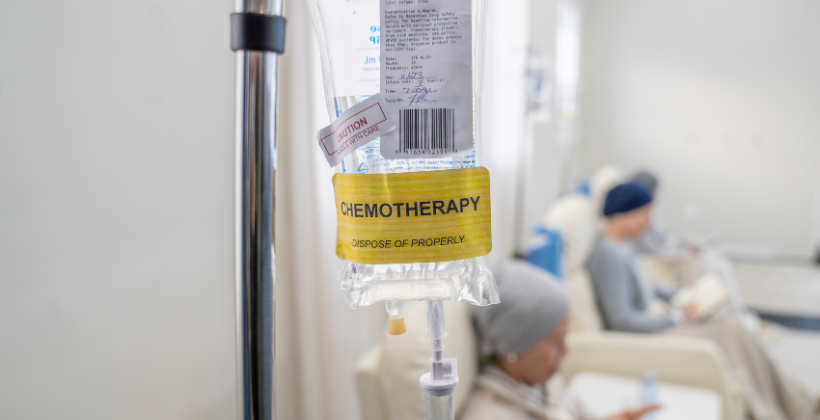
Chemotherapy for Blood Cancer: Understanding Treatment Options, Benefits, and What to Expect
Introduction Getting a diagnosis of blood cancer can change your life, but it’s important to remember that there is real hope with today’s advanced treatments. Chemotherapy for blood cancer is one of the most powerful and widely used treatments. It is very important for killing off abnormal blood cells and improving survival rates. Chemotherapy is often the first thing doctors do to stop leukemia, lymphoma, or multiple myeloma from spreading and get patients ready for other treatments like stem cell transplant. But what does chemotherapy really mean? How long does it take? What are the side effects, and how can you deal with them? This blog will tell you everything you need to know about chemotherapy for blood cancer, such as the different types of treatment available, their pros and cons, and what to expect before, during, and after therapy. The first step to getting better is to understand your treatment journey. We are here to help you every step of the way. What is Blood Cancer and How Does Chemotherapy Help? Blood cancer starts in the bone marrow, blood, or lymphatic system. Blood cancer changes how blood cells are made and how they work, unlike solid tumors. Leukemia affects white blood cells, lymphoma affects the lymphatic system, and multiple myeloma affects plasma cells. These are the three main types. These cancers make it harder for the body to fight infections, move oxygen around, and stop bleeding. Chemotherapy is a major treatment for blood cancer that uses strong anti-cancer drugs to kill blood cells that are growing too quickly. Chemotherapy is usually given systemically, either through oral pills or IV infusions, so it can reach all of the cells in the body that are affected by blood cancer. It helps shrink cancer, bring it into remission, and get the patient ready for a stem cell transplant in many cases. Chemotherapy has a good chance of controlling and curing the disease, especially if it starts early and is done by a professional. It does this by targeting abnormal cells in the blood and bone marrow. Types of Chemotherapy Used in Blood Cancer Chemotherapy for blood cancer isn’t a one-size-fits-all solution. It’s typically administered in carefully structured phases to enhance its effectiveness while reducing the risk of relapse. The treatment plan can differ based on the specific type of blood cancer—like leukemia, lymphoma, or myeloma—as well as factors such as the patient’s age, overall health, and how they respond to the treatment. Here are the main types of chemotherapy protocols that are commonly used: Induction therapy – Induction therapy marks the beginning and most intense stage of chemotherapy for blood cancer. The primary aim here is to swiftly eliminate as many cancer cells as possible and achieve remission. This approach is commonly used for acute leukemia and usually necessitates hospitalization because of the powerful combinations of drugs involved. Consolidation Therapy – Consolidation chemotherapy is meant to get rid of any cancer cells that may still be present but weren’t visible or detectable after the first induction therapy. These cells could cause a relapse. This stage is very important for keeping the remission going. Depending on how well the patient responded, consolidation therapy may use the same chemotherapy drugs as the induction phase or a different set of drugs. The goal is to lower the risk of relapse even more by using high-dose chemotherapy or chemotherapy with other treatments, such as stem cell transplants. Maintenance Therapy: – Taking care of Chemotherapy is usually given for a longer time after induction and consolidation to help keep the cancer from coming back and lower the risk of it coming back. During this phase, the goal is to keep cancer cells from spreading while the patient heals. It usually uses lower doses of chemotherapy drugs and can be given in cycles for months or even years, depending on the type of cancer and the patient’s health. This treatment helps keep any cancer cells that are still there under control. Combination Chemotherapy: – Combination chemotherapy is used to treat a lot of blood cancers, especially leukemia and lymphoma. This means using more than one chemotherapy drug, usually from different classes, that work together to attack different parts of the cancer cell’s life cycle. For instance, in lymphoma, drugs like cyclophosphamide and doxorubicin are used together to attack cancer cells at different points in their growth. Combination therapies are especially helpful for blood cancers because these diseases are so complicated and can become resistant to treatments that only use one drug. Intrathecal Chemotherapy – In some blood cancers, like leukemia, cancer cells can move to the brain or spinal cord. For these kinds of problems, intrathecal chemotherapy is used. This treatment involves putting chemotherapy drugs directly into the cerebrospinal fluid through a lumbar puncture. It helps to find cancer cells in the central nervous system and stop them from spreading. People often use this method with systemic chemotherapy to make sure that cancer cells are killed in every part of the body. Benefits of Chemotherapy Chemotherapy is still one of the best and most common ways to treat different kinds of blood cancer, like leukemia, lymphoma, and multiple myeloma. Chemotherapy for blood cancer has many important benefits that help with recovery and long-term remission when it is given by a qualified hemato-oncologist. This is how it helps: Aims at and kills cancer cells In a systematic way – Chemotherapy works against blood cancers that spread throughout the body because it goes through the bloodstream. This is different from surgeries or localized treatments. It goes after cancer cells wherever they are, but it is most effective in the bone marrow, where abnormal blood cells start to grow. Helps get into remission – Chemotherapy often works to put blood cancer into remission, especially when it is still in its early stages. It cuts down on the number of cancerous cells by a lot, which gives the patient a better chance of living longer and getting better. Gets the body
- admin
- 0 Comments
8 Common Types of Abnormal Menstruation: Symptoms, Causes, and How to Treat Them
Introduction A woman’s menstrual cycle is a good way to tell how healthy she is overall. For some people, their periods follow a set pattern. For others, heavy bleeding, missed periods, or severe pain can make it hard to go about their daily lives. These problems aren’t just small annoyances; they could be signs of health issues that need to be looked into. Understanding the details of your menstrual health is very important because recognizing abnormal menstruation early can help you manage it better and get treatment on time. We at Zynova Shalby Multispeciality Hospital believe in giving women expert care for all aspects of their health, including their menstrual health. In this blog, we’ll look at eight common types of abnormal menstruation, what they feel like, what causes them, and how to treat them. With our medical knowledge, we want to give you the tools to spot possible problems early and get the right care. You can take charge of your health and make sure your periods are healthy and easy to deal with if you have the right information. What is Abnormal Menstruation? Abnormal menstruation is when the menstrual cycle doesn’t follow its normal pattern. This can mean that periods come more or less often, last longer, or are more or less intense. In terms of health, it can include symptoms like heavy bleeding, missed periods, or very bad pain. Most women have a pretty regular 28-day cycle for their periods, but there can be some variation. But if cycles are very different from what is normal, it could be a sign of a health problem. A normal menstrual cycle lasts between 21 and 35 days, and the bleeding lasts for about 3 to 7 days. On the other hand, abnormal menstruation could mean cycles that are much shorter or longer, missed periods, or bleeding that is too heavy or too light. Hormonal imbalances, problems with ovulation, stress, polycystic ovary syndrome (PCOS), thyroid problems, and changes in lifestyle are all common causes of irregular cycles. It’s important to know these things so you can recognize unusual periods and get medical help right away. 8 Common Types of Abnormal Menstruation It’s common for periods to be irregular, but knowing the early signs of abnormal menstruation can help find health problems that may be causing them. There are different kinds of abnormal menstruation, and each one has its own causes and treatments. For example, heavy bleeding and missed periods are two examples. To keep your menstrual health, you need to know about these differences. We will look at 8 common types of abnormal menstruation, their symptoms, causes, and how to deal with them below. A. Menorrhagia (Heavy Menstrual Bleeding) What does Menorrhagia mean? Menorrhagia is when you have very heavy periods that last for several hours and soak through pads or tampons every hour. It is diagnosed when periods last more than 7 days or when you lose more than 80 milliliters of blood each cycle. Common Reasons Fibroids in the uterus Polycystic Ovary Syndrome (PCOS) Problems with the thyroid Endometriosis Signs and Symptoms Symptoms: Frequently soaking through pads, having big blood clots, or feeling tired from losing blood. Treatment: Hormonal therapy or iron supplements are two types of medications that can help. In very bad cases, surgery may be needed to remove fibroids or the uterus. B. Oligomenorrhea (Periods that don’t happen often) What does “infrequent” mean? People with oligomenorrhea have periods less than six times a year, and their cycles are usually longer than 35 days. Common Reason Stress Extreme loss or gain of weight PCOS Problems with the thyroid Signs and Symptoms Symptoms: Long gaps between periods and light bleeding when they do happen. Hormonal therapy or changes to your lifestyle, such as managing stress and changing your diet, can help. C. Amenorrhea (not having periods) There are two types of Amenorrhea primary and secondary amenorrhea Primary Amenorrhea – Primary Amenorrhea: When a girl doesn’t have her period by the time she turns 16. Secondary Amenorrhea – Secondary Amenorrhea is when a woman who used to have regular periods misses three cycles in a row. Common reasons of not having periods Being pregnant Menopause Problems with the pituitary gland A lot of weight loss or exercise Signs and Symptoms Missed periods for a few months are a sign. Treatment Depending on the cause, treatment may include hormonal therapy, lifestyle changes, or treating the underlying condition (like thyroid disorders). D. Dysmenorrhea (Painful Periods) Dysmenorrhea refers to painful periods, which can be either: Primary dysmenorrhea is when you have painful periods that don’t have a medical cause. They usually start a few days before or during your period. Secondary dysmenorrhea is pain that is caused by another condition, like endometriosis, fibroids, or pelvic inflammatory disease. Symptoms Severe abdominal cramps, often starting a day or two before menstruation. Lower back pain, headaches, and fatigue during menstruation. Treatment NSAIDs: Painkillers you can buy without a prescription, such as ibuprofen, can help. Hormonal birth control: to help with pain and keep periods regular. Surgery: If you have severe endometriosis or fibroids, you may need surgery to remove the affected tissue. E. Polymenorrhea (Frequent Periods) : Polymenorrhea refers to menstrual cycles that are shorter than 21 days, resulting in frequent periods. Causes Hormonal Imbalance: When estrogen and progesterone levels are out of whack, it can make cycles shorter. Thyroid Problems: Both hyperthyroidism and hypothyroidism can change how often you get your period. Stress and Changes in Lifestyle: Big changes in your lifestyle or a lot of stress can throw off your period. Treatment Hormonal Therapy: Birth control pills or other treatments that control hormones to keep the menstrual cycle regular. Thyroid Treatment: Medicines that fix problems with thyroid hormones. F. Hypomenorrhea (Light Periods) – Hypomenorrhea is characterized by unusually light bleeding, often lasting less than 3 days. Causes Using birth control pills and IUDs can make your periods lighter. Eating Disorders: Eating disorders like anorexia and severely limiting calories can stop or
- admin
- 0 Comments
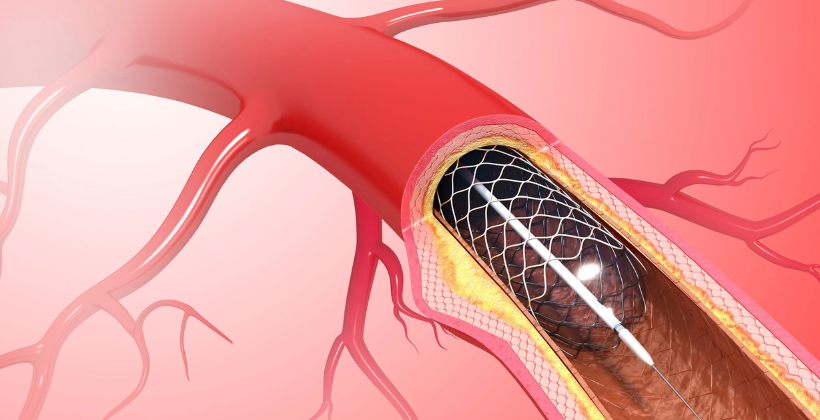
Understanding the Difference Between Angioplasty and Angiography for Heart Care
Introduction Cardiovascular diseases (CVDs) are still one of the most common causes of death around the world, so it’s important to put heart health first. Angioplasty and angiography are two common procedures that can be confusing when it comes to diagnosing and treating heart problems. These terms may sound similar, but they mean different things when it comes to heart care. Knowing the difference can have a big effect on your treatment options. Patients at Zynova Shalby Hospital, which is known for its expertise in cardiovascular care, get the best heart health services available. Angiography is a test that lets doctors see blood vessels to find blockages or narrowing. Angioplasty, on the other hand, is a treatment that opens up these blocked or narrowed arteries so that blood can flow freely to the heart again. Knowing what angioplasty and angiography do can help you make smart choices about your health. We’ll clear up any confusion between the two procedures in this blog and talk about how each one is very important for heart care at Zynova Shalby Hospital. What is Angiography? Angiography is a type of diagnostic imaging that is very important for checking the health of your heart and blood vessels. A special dye (contrast agent) is injected into the blood vessels during angiography. This lets doctors take detailed X-ray pictures. This imaging test gives doctors a clear picture of the coronary arteries and other blood vessels in the body, making it easier for them to find problems like blockages, narrowing, or abnormal blood flow. Angiography’s main job is to find and diagnose problems with coronary artery disease (CAD), which is one of the most common causes of heart attacks and other heart problems. Angiography helps doctors figure out how bad and where the problem is by finding blockages or narrowed arteries. This helps them decide how to treat the problem. This test is especially useful for figuring out what’s wrong with people who have chest pain, shortness of breath, or other symptoms that could be related to heart disease. At Zynova Shalby Hospital, advanced angiography techniques are used to give patients a full picture of their heart health so that they can get the right diagnosis and treatment as soon as possible. How Angiography Works? Angiography is a very useful diagnostic tool that lets doctors see the blood vessels and find any blockages or problems. The process includes putting a contrast dye into the blood, which makes the arteries show up on X-ray pictures. This contrast dye makes it easier to see places where blood flow might be limited or blocked, giving a clear picture of the coronary arteries and other blood vessels in the body. Here’s how the process works: Injection of Contrast Dye: A special dye is put into the blood to make the blood vessels show up on X-ray pictures. Putting in a catheter: A catheter is put into a blood vessel, usually the radial artery in the wrist or the femoral artery in the groin. X-ray Imaging: After the catheter is in place, a contrast dye is injected and X-ray pictures are taken. These pictures show areas of blockages or narrowing in the coronary arteries. Seeing Blockages: The X-ray pictures help doctors find blockages, narrowing, or any other problems in the arteries that could cause heart diseases like atherosclerosis. Precise Diagnosis: These clear pictures help cardiologists figure out exactly what kind of heart disease a patient has so they can suggest the best treatments, like angioplasty or putting in a stent. At Zynova Shalby Hospital, advanced angiography techniques make sure that patients with heart problems get the right diagnosis and the best treatment plans. When Is Angiography Recommended? When there are signs that a person may have a heart condition, doctors usually recommend angiography. It helps doctors look closely at your coronary arteries to find any blockages or other problems. Here are some common reasons why angiography is suggested: Chest pain or discomfort, especially when you’re active or stressed, could mean that blood flow to the heart is low. If you often feel short of breath without doing much, it could mean that your heart isn’t working well. Tiredness or Weakness: If you feel tired for no reason, especially when doing everyday things, it could mean that your heart isn’t getting enough oxygen. Feeling dizzy or lightheaded: These signs could mean that there is a problem with how blood flows through your heart. Feeling dizzy or lightheaded: These signs could mean that there is a problem with how blood flows through your heart. Palpitations or irregular heartbeats: These may be accompanied by chest pain or anxiety and need to be looked into further. Angiography is also recommended in the following situations: 🔍 Possible Coronary Artery Disease (CAD): Based on stress tests, ECG/Echo results, or known risk factors like high blood pressure, diabetes, or high cholesterol. Before heart surgeries like valve replacement, bypass surgery, or angioplasty, doctors check the health of the blood vessels. 🔄 Post-Heart Attack Assessment: To check how badly the arteries were damaged and make plans for more treatment. Angiography gives doctors a clear, detailed picture of what’s going on inside your arteries, which helps them make the best decision for your heart health. What is Angioplasty? Angioplasty is a minimally invasive heart surgery that opens up arteries that have become narrow or blocked, usually because of plaque buildup, which is a condition called atherosclerosis. It’s not a test to find out what’s wrong, but it’s a treatment option that is often done after an angiography shows that there is a blockage in the coronary arteries. Angioplasty’s main goal is to open up the narrowed artery so that more oxygen-rich blood can flow to the heart. This procedure can help with symptoms like chest pain, make the heart work better, and even stop a heart attack in some cases. Angioplasty doesn’t need big cuts like open-heart surgery does. It is done with a catheter that is put in through the groin
- admin
- 0 Comments
Advanced Parkinson’s Disease Treatment by Neurologists in Ghatkopar at Zynova Shalby Hospital
Parkinson’s disease is a progressive neurological disorder that severely impacts an individual’s motor skills and overall quality of life. While there is no cure for the disease, early diagnosis and appropriate treatment can significantly improve symptoms and help patients lead more independent lives. If you or a loved one is dealing with Parkinson’s disease, Zynova Shalby Hospital in Ghatkopar offers comprehensive care and treatment options from experienced neurologists. This blog will dive deep into understanding Parkinson’s disease, its symptoms, causes, and when to consult a neurologist, followed by the advanced treatment options available at Zynova Shalby Hospital. What Is Parkinson’s Disease? Parkinson’s disease is a neurodegenerative disorder that primarily affects Understanding Parkinson’s Disease: Causes and Symptoms the central nervous system, especially the part of the brain that controls movement. The condition occurs due to the degeneration of dopamine-producing neurons, which are responsible for transmitting signals that control movement and coordination. As these cells are lost, the brain’s ability to control and coordinate muscle movements becomes impaired. The disease is most commonly diagnosed in people over the age of 60, though younger individuals can also develop Parkinson’s disease. Men are more likely than women to develop Parkinson’s, and family history plays a role in some cases. While the exact cause remains unknown, researchers believe that genetic and environmental factors work together to increase the risk of the disease. Common Symptoms of Parkinson’s Disease Parkinson’s disease symptoms typically develop gradually and worsen over time. The main motor symptoms include: Tremors: The characteristic shaking of the hands, arms, or legs, often occurring when at rest. Stiffness: Muscles can become stiff or rigid, which leads to a restricted range of motion. Bradykinesia (Slow Movement): Over time, individuals with Parkinson’s disease may experience slowed movements, which can make everyday tasks challenging. Postural Instability: Difficulty with balance and coordination often leads to a higher risk of falls. In addition to motor symptoms, Parkinson’s disease also causes non-motor symptoms, which can have a profound impact on a person’s well-being. These include: Sleep disturbances: Many individuals with Parkinson’s disease experience trouble sleeping, including frequent awakenings and vivid dreams. Mood changes: Depression, anxiety, and apathy are common in people with Parkinson’s. Cognitive decline: Memory problems, difficulty concentrating, and slowed thinking are often seen in advanced stages of Parkinson’s. Causes and Risk Factors While Parkinson’s disease doesn’t have a single identifiable cause, a combination of genetic and environmental factors is believed to contribute to its development. Some factors include: Genetics: Family history can increase the risk of developing Parkinson’s. Several genes have been identified that can influence the likelihood of developing the condition. Environmental triggers: Exposure to toxins, such as pesticides or heavy metals, has been linked to an increased risk of Parkinson’s. Age: The risk of developing Parkinson’s disease increases as people get older, particularly after the age of 60. Gender: Men are more likely to develop Parkinson’s disease than women. When to Consult a Neurologist in Ghatkopar for Parkinson’s Disease If you notice any of the common symptoms of Parkinson’s disease, it’s crucial to seek medical attention from a neurologist in Ghatkopar for an accurate diagnosis. Early diagnosis and intervention can help slow the progression of the disease and improve treatment outcomes. Some early signs that may indicate the onset of Parkinson’s disease include: Subtle tremors: Fine, uncontrollable tremors in the hands, fingers, or legs, especially while resting. Difficulty walking: A noticeable change in walking speed, a shuffling gait, or trouble initiating steps. Reduced facial expressions: Known as a “masked face,” patients may show fewer facial expressions, making it harder for others to read their emotions. Soft or muffled speech: A reduction in the volume or clarity of speech can be an early warning sign of Parkinson’s disease. Importance of Early Diagnosis by a Neurology Specialist Consulting a neurologist as soon as any of the above symptoms are noticed can lead to earlier intervention, which has been shown to improve outcomes for Parkinson’s patients. Early diagnosis allows for more effective symptom management, which can help maintain quality of life. Neurologists at Zynova Shalby Hospital in Ghatkopar use advanced neurological testing, such as MRI scans, PET scans, and dopamine transporter scans, to confirm the diagnosis and develop a treatment plan that is tailored to each patient’s needs. Advanced Parkinson’s Disease Treatments at Zynova Shalby Hospital Zynova Shalby Hospital in Ghatkopar offers cutting-edge treatment options for Parkinson’s disease. The hospital’s neurology department is equipped with the latest diagnostic tools and employs a multidisciplinary approach to treat Parkinson’s patients. Treatment options include medication, surgical interventions, and rehabilitation therapies, all designed to improve patient outcomes. 1. Medication Management The cornerstone of Parkinson’s disease treatment is medication. Levodopa is the most commonly prescribed drug, as it helps replace the dopamine that the brain can no longer produce. Other medications, such as dopamine agonists, mimic dopamine’s effects to help improve motor function. Neurologists at Zynova Shalby Hospital tailor medication regimens based on the patient’s response to treatment, ensuring optimal symptom control. 2. Deep Brain Stimulation (DBS) For patients who no longer respond well to medication or experience severe motor symptoms, Deep Brain Stimulation (DBS) can be an effective surgical treatment. DBS involves implanting electrodes into the brain that deliver electrical impulses to specific areas to regulate abnormal brain activity. This treatment can significantly reduce tremors and rigidity, allowing patients to regain some motor function. The procedure is generally recommended for patients whose symptoms are no longer well-managed by medication alone. 3. Physiotherapy and Rehabilitation Neuro-physiotherapy plays a crucial role in managing Parkinson’s disease. At Zynova Shalby Hospital, patients can benefit from personalized rehabilitation programs that focus on improving mobility, strength, and balance. Physiotherapists help patients with exercises designed to slow the progression of motor symptoms and improve overall functionality. Why Choose Zynova Shalby Hospital for Parkinson’s Disease Care? When it comes to Parkinson’s disease treatment, Zynova Shalby Hospital is recognized as a top neurology hospital in Ghatkopar. The hospital offers comprehensive care, combining state-of-the-art facilities with compassionate,
- admin
- 0 Comments
How ENT Surgery Can Improve Quality of Life for People with Nasal Obstructions
Nasal obstructions can cause a range of symptoms, from chronic congestion to sleep disturbances, affecting daily life. These conditions can impact your ability to breathe properly, sleep well, and even enjoy activities such as eating and exercising. For many, ENT surgery offers a solution to these problems, providing a path to improved quality of life. If you are dealing with chronic nasal blockages or other related symptoms, an ENT specialist in Ghatkopar may be able to help. In this blog, we will explore how ENT surgery can benefit those with nasal obstructions, the conditions that necessitate surgery, and what you can expect during the treatment process. Understanding Nasal Obstructions Before diving into how ENT surgery can help, it’s important to understand what nasal obstructions are and what causes them. A nasal obstruction refers to a blockage or restriction in the airflow through the nasal passages, which can occur due to various reasons, including: Deviated Septum: When the cartilage or bone in the nose is displaced, it can block one or both nostrils, leading to breathing difficulties. Chronic Sinusitis: Inflammation and swelling of the sinus cavities can block the nasal passages, leading to persistent congestion. Nasal Polyps: Noncancerous growths in the nasal passages can obstruct airflow. Allergies: Environmental factors like pollen, dust, and pet dander can lead to inflammation and congestion in the nasal passages. Enlarged Turbinates: These are structures inside the nose that can become swollen, causing blockages. The Role of an ENT Specialist in Ghatkopar An ENT specialist in Ghatkopar is trained to diagnose and treat conditions related to the ear, nose, and throat. When it comes to nasal obstructions, an ENT specialist will first conduct a thorough examination to determine the underlying cause. This may involve using specialized tools like nasal endoscopes or imaging techniques to visualize the nasal passages and sinuses. Once a diagnosis is made, the specialist will discuss treatment options, which may include non-surgical methods like medication or surgery. If you are suffering from chronic nasal blockages that affect your breathing, sleep, or overall quality of life, surgery may be the most effective option to provide long-term relief. How ENT Surgery Can Improve Quality of Life ENT surgery can dramatically improve the quality of life for people struggling with nasal obstructions. The following are some of the key benefits of undergoing ENT surgery: Enhanced Breathing – One of the most immediate and noticeable improvements following ENT surgery is improved airflow through the nasal passages. Whether the obstruction is caused by a deviated septum, nasal polyps, or other structural issues, surgery can help restore proper airflow, allowing patients to breathe freely through both nostrils. This not only improves physical comfort but also enhances overall well-being. Better Sleep Quality – Nasal obstructions can interfere with sleep, leading to problems like snoring, sleep apnea, and frequent awakenings during the night. With improved airflow from ENT surgery, patients often experience better sleep, reduced snoring, and a decrease in sleep apnea episodes. This can result in better rest, more energy during the day, and improved mental clarity and focus. Relief from Chronic Congestion and Sinus Pressure – Chronic sinus congestion and pressure can make everyday activities challenging. Whether it’s feeling constantly congested or dealing with recurring sinus infections, ENT surgery can offer lasting relief by addressing the root cause of these issues. By removing nasal polyps, correcting a deviated septum, or draining blocked sinuses, patients can enjoy improved nasal function and a reduction in sinus-related symptoms. Improved Sense of Smell and Taste – Nasal obstructions can also impair your sense of smell and taste. After surgery, many patients experience a return of their normal senses, which can improve their enjoyment of food and overall sensory experiences. This can be especially important for individuals who have struggled with long-term nasal blockage that has diminished their ability to smell or taste food. Reduced Risk of Recurring Infections – Chronic nasal obstructions often lead to frequent sinus infections or upper respiratory infections. By addressing the underlying issue with ENT surgery, the risk of recurrent infections is greatly reduced. This is particularly beneficial for individuals who are prone to frequent colds, sinusitis, or other upper respiratory problems. Common ENT Surgeries for Nasal Obstructions There are several types of ENT surgery that can help resolve nasal obstructions, depending on the underlying cause of the blockage. Some of the most common procedures include: Septoplasty – Septoplasty is a surgical procedure aimed at correcting a deviated septum, which is one of the most common causes of nasal obstruction. During this procedure, the ENT surgeon straightens the septum to open up the nasal passages, improving airflow and reducing breathing difficulties. Functional Endoscopic Sinus Surgery (FESS) – FESS is a minimally invasive surgery that involves using an endoscope to remove blockages or inflamed tissue from the sinuses. It is commonly used to treat chronic sinusitis, nasal polyps, and other sinus-related issues that lead to nasal obstruction. Turbinate Reduction Surgery – Enlarged turbinates can cause nasal congestion and difficulty breathing. In turbinate reduction surgery, the ENT surgeon removes or reduces the size of the turbinates, allowing for better airflow through the nasal passages. Nasal Polypectomy – Nasal polyps are non-cancerous growths that can block the nasal passages and cause chronic congestion. Nasal polypectomy involves the removal of these growths to improve breathing and alleviate related symptoms. Balloon Sinuplasty – This minimally invasive procedure uses a balloon catheter to expand blocked sinuses, helping to restore proper drainage. Balloon sinuplasty is often used for patients with chronic sinusitis who do not respond to other treatments. What to Expect from ENT Surgery If your ENT specialist in Ghatkopar recommends surgery for your nasal obstruction, it’s important to understand what to expect before, during, and after the procedure. Pre-surgery: Your ENT specialist will conduct a thorough examination and may order imaging tests to assess the extent of your nasal obstruction. You will be given specific instructions on how to prepare for surgery, including fasting and stopping certain medications. During surgery: Most ENT surgeries
- 1
- 2